
Symptomatic treatment is possible with antidepressants and sodium oxybate.
#CATAPLEXY MEDICATION SERIES#
Over time, these severe symptoms evolve to the milder adult phenotype, and this pattern is crucial to recognize when assessing the outcome of uncontrolled case series with potential treatments such as immunomodulation.
Cataplexy shows remarkable differences in childhood compared to adults, with profound facial hypotonia and complex active motor phenomena. Currently, the diagnosis of cataplexy is made almost solely on clinical grounds, based on history taking and (home) videos.

Childhood narcolepsy, with its profound facial hypotonia, can be confused with neuromuscular disorders, and the active motor phenomenona resemble those found in childhood movement disorders such as Sydenham's chorea. They can be differentiated from cataplexy using thorough history taking, supplemented with (home)video recordings whenever possible. Cataplexy mimics include syncope, epilepsy, hyperekplexia, drop attacks and pseudocataplexy. Next to narcolepsy, cataplexy can sometimes be caused by other diseases, such as Niemann-Pick type C, Prader Willi Syndrome, or lesions in the hypothalamic or pontomedullary region. Moreover, childhood cataplexy differs from the presentation in adults, with a prominent facial involvement, already evident without clear emotional triggers ('cataplectic facies') and 'active' motor phenomena especially of the tongue and perioral muscles. The expression of cataplexy varies widely, from partial episodes affecting only the neck muscles to generalized attacks leading to falls. Although cataplexy is rare, its recognition is important as in most cases, it leads to a diagnosis of narcolepsy, a disorder that still takes a median of 9 years to be diagnosed.

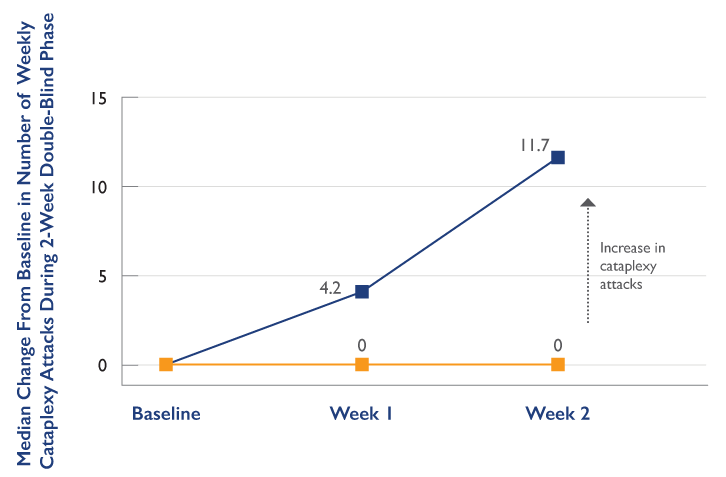
This kind of interprofessional team approach would maximize efficacy and minimize adverse drug reactions of sodium oxybate, translating to enhanced patient outcomes.This review describes the diagnosis and management of cataplexy: attacks of bilateral loss of muscle tone, triggered by emotions and with preserved consciousness. If the poisoning was deliberate, referral to a psychiatrist is required. As depicted above, it is the responsibility of the entire healthcare team, such as clinicians (MDs, DOs, NPs, PAs), nurses, specialists, and pharmacists, to work in close collaboration. The medical toxicologist can assist if multiple drug ingestions are suspected. Critical care physicians ensure proper care of intubated patients. In overdose, emergency department physicians and triage nurses should stabilize the vitals. The program focuses on limiting drug distribution and educating patients on the proper use of the drug. An extensive risk management program from the drug manufacturer can help to prevent the misuse of sodium oxybate. Concomitant use of CNS depressant and the patient’s health history resulted in an unintentional overdose. Specially trained nurses can monitor for the signs of improvement and should inform the prescriber of any discrepancies. Furthermore, nurses can reinforce the importance of strict adherence to the treatment regimen.Ī 2009 forensic multi-drug intoxication fatality involving sodium oxybate presented a sleep apnea patient who had mistakenly received prescriptions for various CNS depressants, including sodium oxybate. Pharmacists should also counsel in detail regarding the potential adverse drug reactions. Pharmacists should ensure proper dosing and step-by-step instruction on taking sodium oxybate to minimize adverse events.

Sodium oxybate is usually prescribed for narcolepsy by a board-certified sleep medicine physician or neurologist. Prescribers need to be cautious when prescribing a Schedule III controlled substance such as sodium oxybate due to the high potential for abuse.


 0 kommentar(er)
0 kommentar(er)
